PTH Effects on Bone
PTH has a rapid effect (occurring within minutes), whereby it stimulates osteoblasts to pump Ca++ ions out of the fluid surrounding the bone (which has a higher Ca++ concentration) and into the ECF. Over a longer time course, PTH stimulates bone resorption. Although PTH stimulates bone resorption, it is actually the osteoblasts that express PTH receptors. PTH stimulation of osteoblasts causes them to express a signaling molecule that activates osteoclasts. For more details, see the page on bone remodeling.
PTH Effects on Kidney
PTH has two important effects on the kidney that work to increase [Ca++]ECF. First, it decreases the loss of Ca++ ions in the urine by stimulating Ca++ reabsorption. "Reabsorption" is the term used to describe the transfer of substances from the forming urine back into the ECF. Filtration, the first step in urine formation, is a nonspecific process, whereby water and low molecularr weight substances move by bulk flow from the plasma and into the forming urine. Reabsorption, which is performed by the cells of the kidney tubules, allows the recovery of those useful small molecules such as sugars, amino acids, and Ca++ ions. As well as stimulating Ca++ reabsorption, PTH also inhibits phosphate reabsorption.
The other key effect of PTH on the kidney is to stimulate production of 1,25(OH)2D, the active form of vitamin D. Vitamin D3 is synthesized in a photochemical reaction in the skin, in response to sunlight. Vitamin D3 and a similar compound derived from plants are present in foods; collectively these are referred to as vitamin D. A constitutively active enzyme in the liver produces 25-(OH)D. The role of PTH is to stimulate the kidney enzyme, resulting in the production of 1,25(OH)2D. This is extremely important for bone health and Ca++ homeostasis because 1,25(OH)2D works in the small intestine to promote Ca++ absorption.
In kidney disease, inadequate amounts of 1,25(OH)2D are made. What happens is that Ca++ homeostasis is maintained at the expense of bone. [Ca++]ECF drops because of a lack of Ca++ absorption from the diet. Hypocalcemia stimulates high levels of PTH secretion; this is termed secondary hyperparathyroidism because the problem that causes the hyperparathyroidism is in the kidney, not at the parathyroid gland. Secondary hyperparathyroidism is treated by administering vitamin D and Ca++ supplements. The drug cinacalcet has recently been approved for the treatment of secondary hyperparathyroidism. Cinacalcet is a calcimimetic drug that binds to the Ca++ receptor on cells in the parathyroid gland, inhibiting the secretion of PTH.
http://courses.washington.edu/conj/bess/calcium/calcium.html

Figure 1
Interrelationships among FGF23, PTH, 1,25(OH)2D, and Klotho.
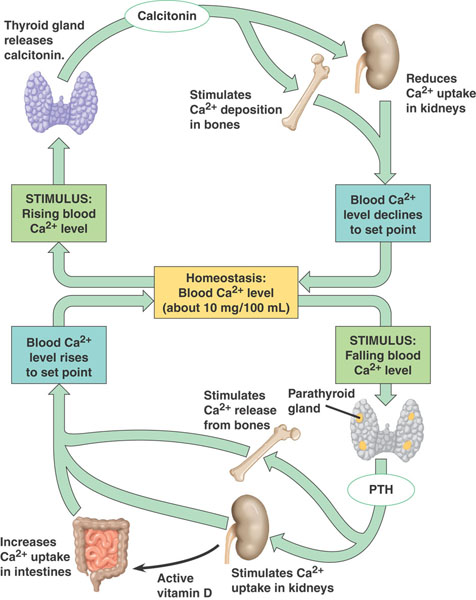
(A) The PTH/1,25(OH)2D axis. The principal function of the PTH/1,25(OH)2D axis is to regulate calcium homeostasis. Decrements in serum calcium levels stimulate PTH secretion by the PTG, which targets the kidney to reduce urinary calcium excretion, stimulate 1α-hydroxylase activity, and enhance the fractional excretion of phosphate (PO4), and targets bone to increase the efflux of calcium and phosphate. The resulting increase in 1,25(OH)2D targets the gastrointestinal tract to increase dietary absorption of calcium, which suppresses PTH. (B) The FGF23/Klotho axis. FGF23 produced by bone principally targets the kidney, leading to reductions in serum phosphate and 1,25(OH)2D levels by stimulating the fractional excretion of phosphate and reducing 1α-hydroxylase activity. The receptor for FGF23 in the kidney is a Klotho:FGFR1 complex located in the distal tubule. There may be a distal-to-proximal feedback mechanism that mediates the effects of FGF23 on the proximal tubule. FGF23 also decreases the kidney expression of Klotho, which diminishes renal tubular calcium reabsorption via its interactions with transient receptor potential cation channel, subfamily V, member 5 (TRPV5). FGF23 may also directly target the PTG to reduce PTH secretion. FGF23 is the principal phosphaturic hormone and may function to counter the hypercalcemic and hyperphosphatemic effects of excess 1,25(OH)2D through reductions in PTH and elevations in FGF23 levels.
http://www.jci.org/articles/view/36479/figure/1
Comments (0)
You don't have permission to comment on this page.